Opioid Stewardship Programs in Rural Arizona
New Resource Available
Harnessing the Power of Rural
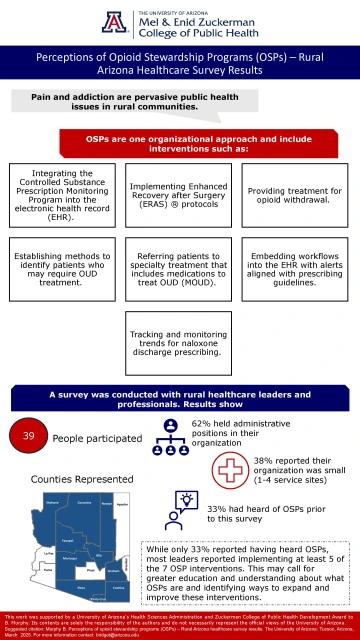
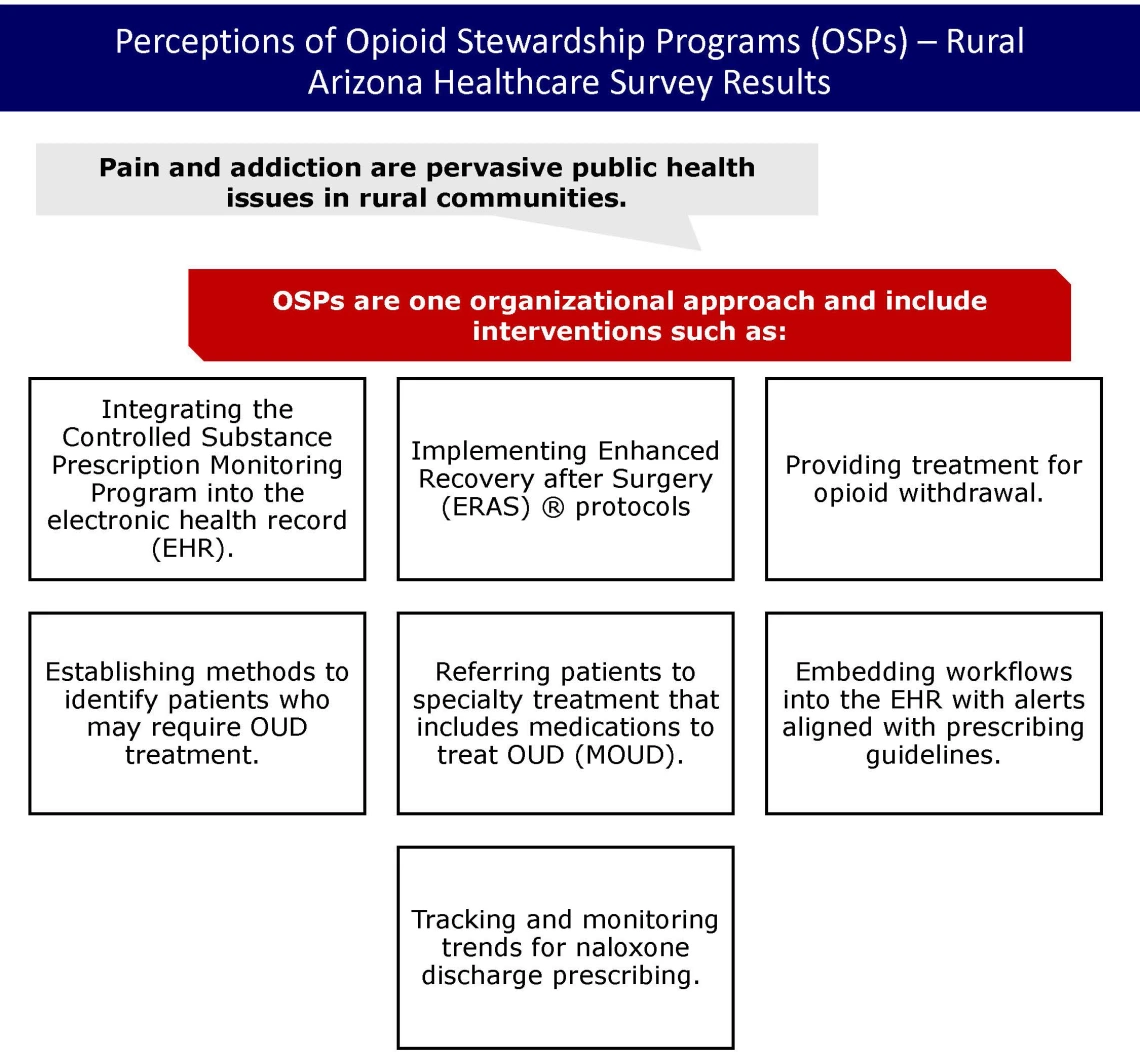
Pain and substance misuse and addiction continue to be public health priorities. Rural, underserved, and under resourced populations consistently show dissimilarities in healthcare access, quality, and outcomes. Yet, as revealed by recent research findings, rural hospitals harness the available resources to provide services and support to address pain and addiction.
Opioid Stewardship Programs (OSPs) are a suite of tools to address substance misuse. Dr. Bridget Murphy, Assistant Research Professor at the University of Arizona Mel and Enid Zuckerman College of Public Health, aims to advance OSPs in rural areas. With the support of the University of Health Sciences Career Development Award mentoring team, Dr. Murphy continues to build on previous research, developing strategies to advance OSPs in rural areas.
Findings from a recent survey of rural healthcare leaders and professionals on Opioid Stewardship Programs (OSPs) builds on evaluation conducted in 2020. The 2020 evaluation, led by Dr. Benjamin Brady surveyed hospital administrators, in both the emergency department and acute care settings, about their level of implementation on 11 OSP interventions. The team found some level of OSP implementation in nearly every hospital.1 Dr. Murphy’s research furthers this work by conducting surveys with rural healthcare leaders and professionals about OSPs in rural healthcare, and developing an implementation guide for rural hospitals. The team is seeking continued funding for this work.
Basic Results of the Survey
There were 39 people who completed the survey. Participants represented 10 of the 15 Arizona counties. Most (62%) held administrative positions and 38% reported their organization was small (1-4 service sites). Thirty-three percent reported hearing about OSPs prior to conducting the survey.
Next Steps
Thirty-three percent of the survey participants indicated they had heard of OSPs prior to the survey. While this may seem low, most participants who identified as leaders indicated their organization implements at least 5 of the 7 OSP interventions. This study tells us that rural healthcare organizations implement OSP interventions and there may be opportunities for continued education and support for implementation.
Resources:
To learn more about pain and addiction:
- 2022 CDC Clinical Practice Guideline https://www.cdc.gov/overdose-prevention/hcp/clinical-guidance/index.html
- American Society of Addiction Medicine’s Clinical Guidelines https://www.asam.org/quality-care/clinical-guidelines
- Arizona Pain and Addiction Curriculum https://www.azdhs.gov/audiences/clinicians/arizona-pain-addiction-curriculum/index.php
Recorded Asynchronous Trainings
Arizona Center for Rural Health Webinar Series. See relevant trainings in the archive of past webinars here: https://crh.arizona.edu/events/center-rural-health-webinar-series
Comprehensive Center for Pain and Addiction. Cannabis Education for Health Professionals. https://www.eventbrite.com/e/cannabis-education-for-healthcare-professi…
Western Region Public Health Training Center. Sign in or create an account to find these and many other trainings: https://moodle.publichealth.arizona.edu/login/
- Enhancing Care for Opioid Use Disorder through Collaborative Training (2024)
- Enhancing Treatment for Chronic Pain: Opioids and Complementary Care (2023)
- A New Era of Treatment for Substance Use/Opioid Use Disorder (2023)
- Integrating Care: Advancing Health Equity through Whole-Person Responses to Pain and Addiction (2023)
- Opioid Stewardship Programs: An Organizational Strategy for Addressing Pain and Addiction (2023)
- Overdose recognition and naloxone administration training (English) (2023)
- Overdose recognition and naloxone administration training (Spanish) (2023)
References
1. Brady B, SantaMaria B, Ortiz y Pino K, Murphy B. Opioid stewardship program implementation in rural and critical access hospitals in Arizona. J Opioid Manage. 2024;20(1):21-30. doi:https://doi.org/10.5055/jom.0842
2. Santalo O. Before it is too late: Implementation strategies of an efficient opioid and pain stewardship program. Am J Health-Syst Pharm. 2020;77(8):636-643. doi:10.1177/0018578719882324
3. Shrestha S, Khatiwada A, Sapkota B, et al. What is “Opioid Stewardship”? An overview of current definitions and proposal for a universally acceptable definition. J Pain Res. 2023;16. doi:https://doi.org/10.2147/JPR.S389358
4. Dowell D, Ragan K, Jones C, Baldwin G, Chou R. CDC clinical practice guideline for prescribing opioids for Pain — United States, 2022. MMWR Recomm Rep. 2022;2022(71(No. RR-3)):1-95. doi:http://dx.doi.org/10.15585/mmwr.rr7103a1
5. Grant MC, Chappell D, Gan TJ, et al. Pain management and opioid stewardship in adult cardiac surgery: Joint consensus report of the PeriOperative Quality Initiative and the Enhanced Recovery After Surgery Cardiac Society. J Thorac Cardiovasc Surg. Published online January 28, 2023:S0022-5223(23)00089-2. doi:10.1016/j.jtcvs.2023.01.020